Researchers from the University of Wollongong (UOW) in Australia have developed a custom 3D bioprinter dedicated specifically to treating microtia, a congenital deformity that results in an underdeveloped external ear. The bespoke bioprinter, named 3D Alek, was recently installed at the Royal Prince Alfred Hospital (RPA) in Sydney.
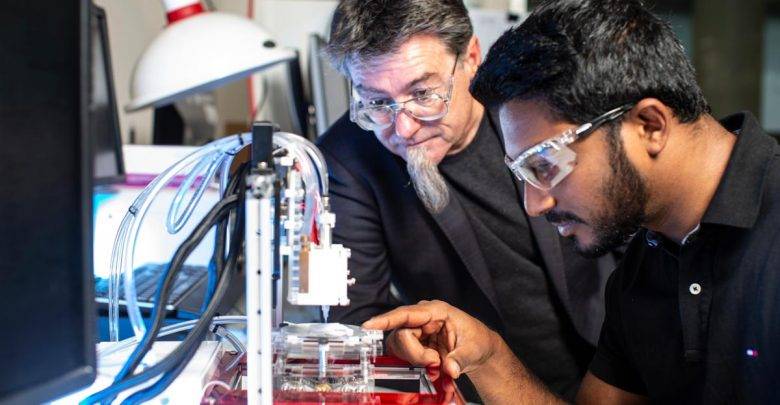
The 3D Alek bioprinter was developed by a UOW team working at the ARC Centre of Excellence for Electromaterials Science (ACES) in collaboration with associate professor and Ear, Nose and Throat (ENT) surgeon Payal Mukherjee. Together, they sought to find a clinical bioprinting solution to microtia, a rare condition that only about a dozen or so babies are born with a year in Australia.
By combining their respective expertises, the researchers and surgeon were able to come up with the 3D Alek, a custom, multi-material bioprinter that uses a specialized bioink to help in the regeneration of cartilage for reconstructive ear surgery. The bioink in question was also developed by ACES researchers at UOW with help from the Australia National Fabrication Facility (ANFF).

“This project illustrates our ability to manage a successful pipeline to turn fundamental research into a strategic application to create a new health solution to improve people’s lives,” said ACES Director Professor Gordon Wallace. “We have been responsible for the primary sourcing of materials; the formulation of bio-inks and the design and fabrication of a customized printer; the design of required optimal protocols for cell biology; through to the final clinical application.
“With one 3D Alek now established in a clinical environment at RPA and a replica in our lab at TRICEP, our new 3D bioprinting initiative, we will be able to fast-track the next stages of our research to deliver a practical solution to solve this clinical challenge.”
The bioprinter will enable medical professionals at the RPA hospital in Sydney to come up with patient-specific treatments to microtia and enable them to reproduce the complex geometry of an external ear.
“Treatment of this particular ear deformity is demanding because the outer ear is an extremely complex 3D shape, not only in length and breadth, but also in height and projection from the skull,” Professor Mukherjee said. “This is where bioprinting is an extremely exciting avenue, as it allows an ear graft to be designed and customized to the patient’s own face using the patient’s own natural tissue—resulting in reduced operating time and improved cosmetic outcome—and avoids the current complication of requiring a donor site for cartilage, usually from the patient’s rib cage.”
With the 3D Alek bioprinter installed at the RPA hospital, the joint team will continue its bioprinting for microtia research. The next step will involve early clinical trials aimed at accelerating the development of the bioinks by using stem cells from human tissue. The ultimate goal is to 3D print a living ear using a patient’s own stem cells.
The university of Wollongong has established itself as a leader in bioprinting technologies. In fact, the Australian university even offers a free online course teaching the fundamentals of the technology. Famously, the university developed the 3D BioPen, a unique device that “draws” stem cells to regenerate cartilage.
Source: 3dprintingmedia.network