A new study conducted at the University of Oxford offers significant progress in using 3D-printed neural tissues to repair brain injuries.
Brain injuries, including traumatic brain injury (TBI), may seriously damage the brain’s cerebral cortex, or its outer layer of nerve cell tissue. The cerebral cortex carries out essential, complex processes of the brain such as thought, memory, and motor functions. It consists of six layers of neurons, the basic building blocks of the nervous system, responsible for carrying and transmitting information throughout the body. Injury to different areas of the cerebral cortex may produce varying physical, emotional, or cognitive effects.
A few causes of brain injury include stroke, brain tumours, and disease. TBI refers to serious head trauma caused by an external force. It disrupts brain function and remains a global public health problem, affecting approximately 70 million people worldwide. Despite being a leading cause of injury-related death or disability, pharmaceuticals and biotherapeutics have not offered an effective treatment for severe brain injuries.
Tissue regenerative therapies using stem cells are a potential treatment for brain injuries, yet stem cells have still not successfully replicated the complex structure of the brain. The researchers instead used a droplet printing technique to imitate and 3D print a simplified, two-layer version of the cerebral cortex’s six-layer cellular architecture.
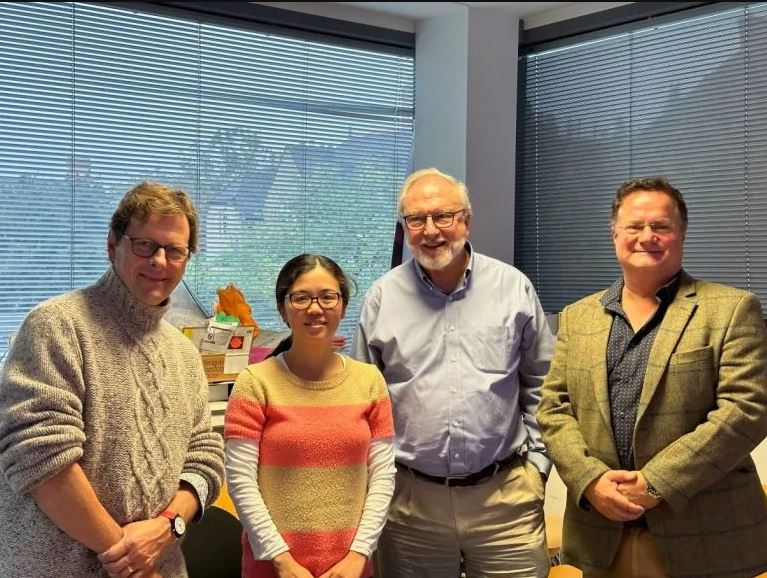
The project began in late 2020 when senior authors Dr. Linna Zhou (Department of Chemistry), Dr. Francis Szele (Department of Physiology, Anatomy and Genetics), Dr. Zoltán Molnár (Department of Physiology, Anatomy and Genetics), and Dr. Hagan Bayley (Department of Chemistry) came together via the Oxford Martin Programme on 3D Printing for Brain Repair. The programme has funded and supported the project, allowing collaboration with students and postdoctoral researchers.
Dr. Yongcheng Jin (Department of Chemistry) is the lead author of the project. In an emailed statement, Dr. Jin said he is very passionate about regenerative medicine and that the team was amongst the first groups working on 3D bioprinting. The project didn’t garner much attention in its initial stages, he added, but it is now being more widely recognised.
Through pooling together their varying expertise, the group established a unique 3D printing technique that was biocompatible with human neurons. In an interview with the senior authors, Dr. Bayley said when the team began 3D printing, no one had done it the way they had.
“We printed various small droplets in the picolitre range, where a picolitre is 10-12 litres, so getting down towards cell size”, he added. “So, we can take different types of cells and use the 3D printing method to print them in very high resolution.”
The development in 3D printing likewise represents massive progress in engineering human cortical columns. Human induced pluripotent stem cells (hiPSCs) were printed to replicate cerebral cortical tissue with a two-layer design. The two layers represent the upper and lower cortical layers. The brain cannot repair itself, so using stem cells enables the replacement of nerve cells lost to disease or injury.
Stem cell treatments involving early human embryonic cells have been met with ethical concerns. Collecting embryonic cells risks killing the embryo, thereby making it a controversial practice, particularly amongst some religious groups. The study bypasses this controversy through using hiPSCs, which are easily obtained through skin cells, blood cells, or even air cells. Dr. Szele said hiPSCs can replicate the early embryonic stem cells which are in a state of totipotency. This means the stem cells can generate almost any cell in the body.
After printing the simplified cerebral cortical column, it was implanted into ex vivo mouse brain slices. The implantation resulted in significant integration between the implant and host tissue.
“The tissue can form cross-processes into the brain slices”, Dr. Zhou said. Thus, neurons crossed the implant-host boundary and the implanted human cells communicated with the mouse cells.
The researchers plan to continue their work with droplet printing in hopes of engineering a more accurate cerebral cortical tissue.
“We don’t know whether it is really functional repair yet, but they influence the host tissue”, Dr. Molnár said. “So the long term goal is to perfect this construct, which will integrate extremely well and better than the associated cells … and eventually improve the host condition.”
This project marks a milestone in the path to personalised implantation treatments for brain injuries. When discussing the possibility for implantation to be a low-cost treatment, the authors noted the commercialisation of stem cell technologies will drive down its costs. Dr. Jin said partnerships, subsidies, or alternative funding bodies may facilitate the commercialisation process to make personalised treatments more affordable.
The future of 3D printing in medicine holds great promise. It can potentially be used for drug screening, personalised prosthetics, organ repair, and much more.
Nonetheless, this is still a work in progress, and the long-term goal of neuron repair through stem cells and bioprinting techniques is still in its infancy. In fact, all cells in the human body have yet to be identified. While other scientific developments are occurring in parallel, the team still has a long road ahead in refining their method.
“This is just the beginning”, Dr. Molnár said. “These paradigms that we are doing now, 30 years ago, were a dream.”
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com