Researchers at the Indian Institute of Technology (IIT) Delhi have successfully 3D bioprinted human skin models that have certain anatomically relevant structural, mechanical and biochemical features similar to native human skin. The bioprinted skin produced in the lab by the team is already being used by ITC Ltd for experiments.
The bioprinted skin model will have wide applications in testing cosmetics. It can also reduce and probably even replace testing on animals.
It can also be used for testing dermatology drugs on human skin and at a future date even help in testing drugs for personalised medicine.
Testing on animals
The European Commission has prohibited testing finished cosmetic products and cosmetic ingredients on animals. It even prohibits marketing of finished cosmetic products and ingredients in the European Union. The skin is composed of two important layers — the inner dermis (made of fibroblasts) and the outer epidermis (keratinocytes, melanocytes). The junction between the two layers is not flat but is undulatory or wavy. The undulatory morphology is important as it provides biochemical cues and mechanical support to the epidermis layer, provides structural stability to the skin by making the two layers adhere to each other, and not allow cells to cross the junction.
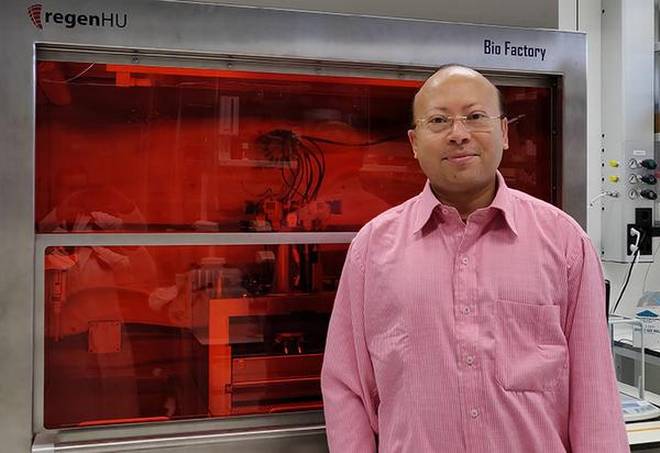
Unlike the currently available tissue-engineered skin equivalents, the team led by Sourabh Ghosh from the institute’s Department of Textile Technology was successful in creating this wavy junction in the bioprinted skin model. The results were published in the journal Bioprinting. The study was funded by ITC Ltd.
The undulatory junction was designed using 3D CAD and 10 layers of dermis were constructed through bioprinting followed by eight layers of epidermis. “We designed the pattern so that both layers fit and the interface had a wavy pattern,” says Prof. Ghosh. Silk bioink mixed with fibroblasts was used for growing the dermis, while bioink mixed with keratinocytes and melanocytes was used for growing the epidermis.
No shrinkage
The bioprinted skin also retained the original dimension without any shrinkage for up to three weeks. Traditionally, collagen used for developing skin constructs start shrinking within a few weeks thus affecting the morphology. Testing on such skin constructs therefore cannot be carried out beyond one week.
The bioink containing the cells are deposited in a criss-cross pattern leaving gaps in between. “The keratinocytes in the epidermis were seen migrating and filling the pores. This type of migration, which was very clear and striking, and cellular self-assembly recapitulate wound healing-like situation in native skin,” says Prasad Admane from IIT Delhi and first author of the paper.
The keratinocytes in the epidermis differentiate and form into four distinct layers. “We studied three proteins — fibronectin, cytokeratin 1 and 14 — that are biomarkers of keratinocyte differentiation. They are produced in the bioprinted skin though the amount was comparatively less than native skin,” he says.
Most importantly, gene and protein expression analysis showed 60% similarity in gene expression between bioprinted and native skin. “We identified 56 proteins expressed in bioprinted skin which play an important role in skin development, extracellular matrix organisation and keratinocyte differentiation,” says Abhishak C. Gupta from IIT Delhi and co-author of the paper.
“We will now explore the possibility of growing hairs on the bioprinted skin,” says Dr. Gupta.
Prof. Ghosh’s team has already developed a 3D construct for hair follicle structure in collaboration with ITC Ltd.
“Our goal is set up a start-up to focus on developing different diseased skin conditions to test different drug molecules in patient-specific manner,” he says.