Credit: www.theneweconomy.com
When two NASA employees created the first affordable 3D printer prototype in 2013, enthusiasm from all sectors reverberated around the globe. For medical practitioners, the idea that 3D printers could be used to build human organs became the ultimate goal.
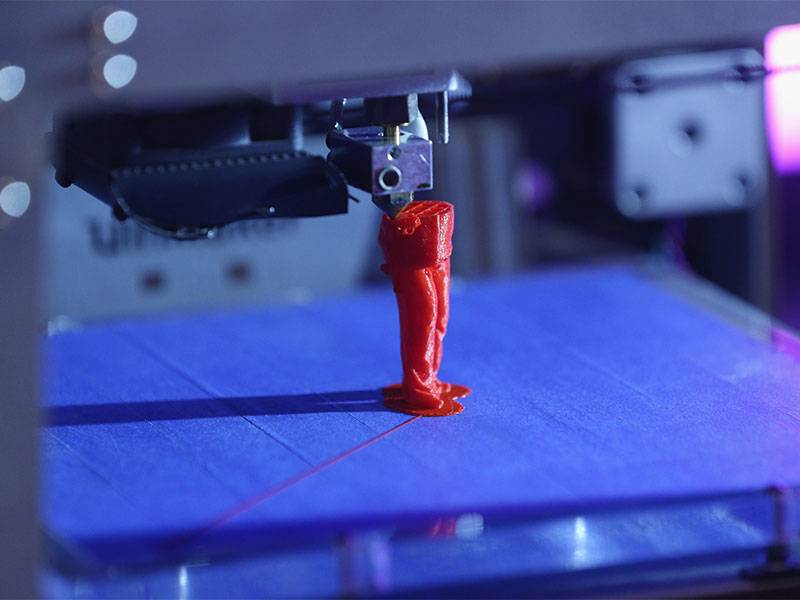
The 3D printer first took form in 1984 when Charles ‘Chuck’ Hull filed a patent for stereolithography technology, which is used for 3D printing in the layer-by-layer method that is so recognisable today. The technique uses photopolymerisation, a process through which light links molecules together, forming polymers. This first generation of 3D printers, however, used materials that were not robust enough for final products, limiting them to rapid prototyping.
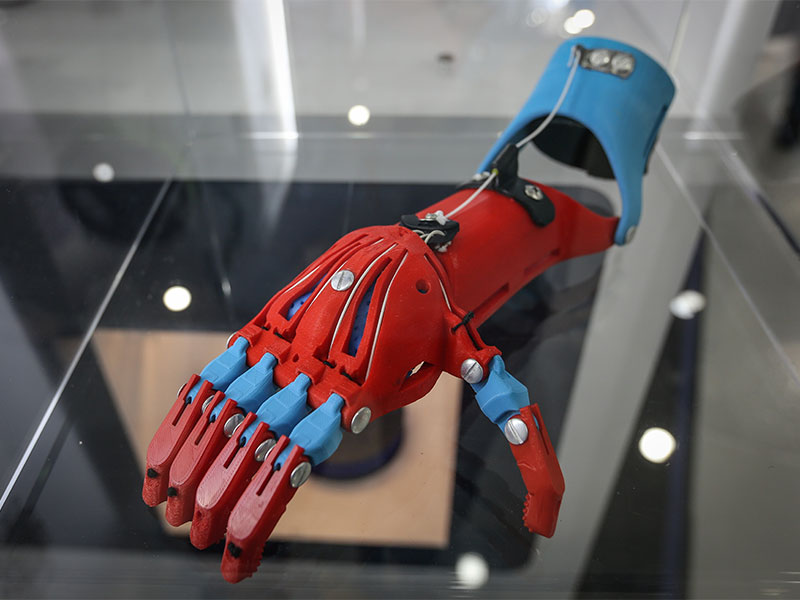
Around a decade later, Hull’s company, 3D Systems, introduced nanocomposites, a new generation of materials for 3D printing. Made of blended plastics and powdered metals, they were far more durable than their predecessors, opening the door to 3D printing for durable end-products. The medical sector soon came calling.
Over the following years, new processes and techniques were developed, paving the way for 3D printed organs. A seminal moment came in 1999 when scientists at the Wake Forest Institute for Regenerative Medicine printed an artificial scaffold of a human bladder. Once covered in human cells, the scaffold was able to grow working organs; the stage for bioprinting was set.
Bringing organs to life
Numerous milestones have been met since then: in 2002, functional (though miniature) kidneys were transplanted back into animal subjects, and in 2010 the first blood vessel was printed. Progress has been slow, but for good reason: while bioprinting can successfully create human skin, cartilage and retinas, it can only do so because such tissue is very thin, small or devoid of blood vessels.
Zhengchu Tan, a researcher at Imperial College London’s Department of Mechanical Engineering, explained the challenge facing scientists: “In order to 3D print a full organ, all the different cells that are found in the organ must be implanted or derived from stem cells.
These cells must then create the complex biological structure of the organ, including the arrangement of blood vessels (vasculature). Then we need to test whether the organ is able to complete its normal function in the body.”
Fortunately, the field has seen significant developments of late. Scientists at United Therapeutics, a biotech company based in Maryland, US, are working on a printer that could recreate the intricate details that make up a lung, including all 23 branches, as well as accompanying alveoli and capillaries.
United Therapeutics is using a collagen printer made by 3D Systems, and is also working with start-up firm 3Scan to create detailed maps of the structure of lungs. So far, United Therapeutics has printed just a few branches with no cells, but there’s a great deal of enthusiasm that an entire lung could be possible in a decade or so.
To make that happen, the company must overcome the challenge of resolution size. At present, 3D Systems’ printer can achieve a resolution of 20 micrometres. A lung, however, will require components less than a micrometre in size.
According to an interview with MIT Technology Review, Pedro Mendoza, Director of Bioprinting at 3D Systems, said he plans to use techniques from the semiconductor industry, such as mirrors, masks and lasers, to improve the resolution size currently being achieved.
Speed also needs to be addressed – at the current rate, a completed lung scaffold would take around a year to build – while bringing the matrix to life is another challenge.
“There’s a great deal of enthusiasm that an entire lung could be possible in a decade or so”
San-Diego-based Organovo – which is, incidentally, the company that created the first 3D printed blood vessel – has been making strides in the field too. The company has developed a process that can turn cells from donor organs into printable ‘bioink’.
Layers are then printed to build sections of liver tissue, which Organovo plans to use for clinical trials – a welcome alternative to animal testing. It has also started helping patients directly: as of December 2017, Organovo was given orphan drug designation to treat a rare condition, alpha-1 antitrypsin deficiency, using its 3D printed liver tissue.
Blood runs cold
Imperial College London, in collaboration with King’s College London, meanwhile, is approaching the task by using cryogenics to create 3D printed structures. Tan, one of the scientists working on the project, told The New Economy how the technique works: “The printing material is a liquid solution. To turn it into a soft, solid material, it must be frozen and then thawed. This is where we use cryogenics to freeze the printing solution, hence solidifying it.”
By using this method, the team is able to create structures that can imitate the characteristics of organs. Tan added: “By solidifying each layer, further layers can be built on top to create 3D structures. After the frozen structure is created, it is thawed and it turns into a super-soft hydrogel that mimics the mechanical properties of the brain.”
Structures made from hydrogels can be used to create scaffolds, which act as templates for tissue regeneration. This method allows cell regeneration without the issues often associated with tissue transplants – namely, rejection.
That said, hydrogel structures come with their own issues. “One of the main challenges of 3D cell culturing is that cells seeded deep inside a cell seeding substrate cannot survive if there is an inadequate flow of cell culture medium,” Tan explained. This includes oxygen, water and nutrients.
Fortunately, cryogenic 3D printing can solve this problem. The system is able to create hollow structures, meaning the cell culture medium can flow through the entire structure. “This brings the research closer to achieving full 3D tissue regeneration,” Tan explained. “The 3D scaffold also provides a structure that the cells can grow on to aid the development of their own extracellular matrix and eventual shape, instead of growing from
a flat 2D petri dish.”
She added: “The cryogenic technique is unique because it utilises the liquid to solid phase change of the printing ink in order to build up layers in 3D. The printing material is able to crosslink after the frozen structure is thawed, which means that no toxic chemicals (crosslinking agents) or harsh UV radiation (photocrosslinking) that might harm cells are required. This makes the technique very friendly to cells and tissue regeneration, as cells are often frozen and thawed for storage.”
Printing on the brain
While the team at Organovo works to increase the size of tissue it can grow, United Therapeutics is trying to circumvent the current limits of printing resolution. For the team at Imperial College London, meanwhile, research is now focused on improving the cryogenics system to print much larger and more complex structures.
“There has also been a development on the composite hydrogel printing material: it has been formulated to mimic [the] brain, lung and liver so we will be able to print structures that mimic various organs,” Tan said.
“The main application for these structures is to provide a more accurate in-vitro testing method and a more ethical alternative to animal testing for destructive cell studies (chemo, radio and immunotherapy). Specifically, the end goal will be to study how different brain tumour cells respond to different lines of treatment. The ultimate goal will, of course, be to create a full human artificial brain.”
There is still a long way to go until organs can be printed on a large scale, eradicating fatally long waiting lists and unnecessary deaths as a result. But developments are being made and the scientists working on them are incredibly committed. Whether using cryogenics or printable bioink, it seems certain that 3D printed organs will be brought to life.