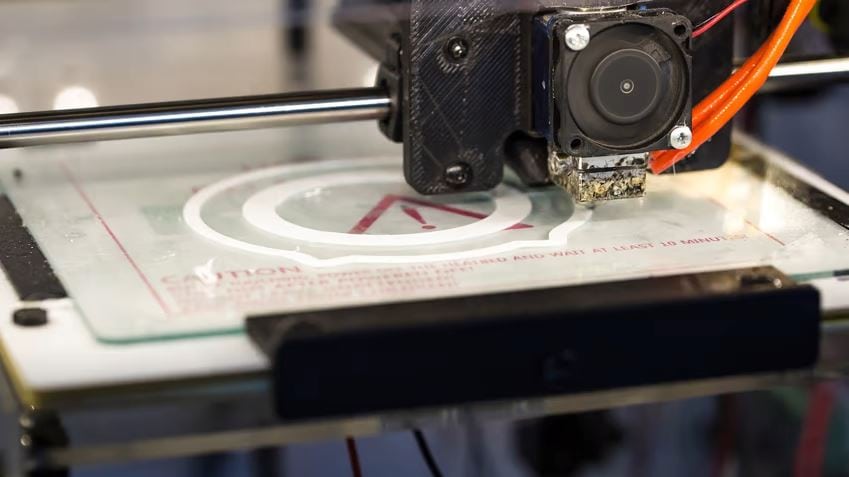
The FDA has begun outlining a potential approach for regulating a cutting-edge front emerging in healthcare: the 3D printing of medical implants or devices customized for each individual patient and manufactured on-site and on-demand within hospitals or doctor’s offices.
More from the News
This technology could one day provide specific spine implants designed to fit perfectly among a particular patient’s vertebrae or quickly build accurate, physical models that surgeons could use to help plan out and rehearse a risky procedure, according to the agency.
Starting with a published discussion paper, the FDA is now collecting comments from the medtech industry and the public to help inform future guidance documents. The agency is seeking input on which of today’s regulations, aimed at so-called traditional device manufacturers, would be easy or difficult for 3D-printed devices to satisfy, among other topics.
“The 3D printing of medical devices is at the forefront of innovation and healthcare,” the FDA’s William Maisel and Ed Margerrison, directors of the Office of Product Evaluation and Quality and the Office of Science and Engineering Laboratories, respectively, said in an agency statement.
“The discussion paper we’re sharing today provides insight into our perspective of the benefits and challenges of 3D printing at hospitals and other points of care and presents a potential approach for regulatory oversight under various scenarios to inform future policy development,” Maisel and Margerrison added.
“This feedback will help build the foundation for an appropriate regulatory approach for 3D printing at the point of care, personalized care for patients and new innovations in this area,” they said. The FDA previously issued guidance on 3D-printed products manufactured outside the point of care in December 2017.
The new discussion paper outlines a number of future scenarios—such as a hospital maintaining its own medical device production system. Generally, the FDA said, a point-of-care 3D-printing facility would not be considered a manufacturer by itself if the company demonstrates that multiple raw materials, scanners or printers could consistently produce high-quality devices.
However, some exceptions to that rule may occur if certain post-processing actions are taken within the hospital, such as machining, drilling or sterilization steps that may affect a product’s safety or effectiveness.
Other examples include 3D-printing facilities maintained by the company near the healthcare provider to produce patient-matched titanium implants or specially designed prostheses. Between both settings, certain regulatory responsibilities would have to lie with the company, and others with the healthcare facility, the agency said.
The FDA is also asking for feedback on which types of 3D-printed devices would produce the lowest risk to the patient and what regulatory flexibility the agency could provide in that space. Submissions are being collected through February 8, 2022.
In addition, the agency is looking to learn how 3D printing has been employed over the course of the COVID-19 pandemic, including new situations and product shortages where users may not have had all the information they needed.
In March 2020, as the demand for critical medical hardware began to outpace supplies worldwide, 3D printers were seen as a way to quickly produce scarce ventilator valves and other parts, as well as personal protective equipment such as face masks and rigid plastic shields.
The FDA began working with a range of public and private organizations to evaluate and distribute 3D designs and models alongside the National Institutes of Health, the Department of Veterans Affairs and America Makes, the national accelerator program for additive manufacturing managed by the Department of Defense.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com/