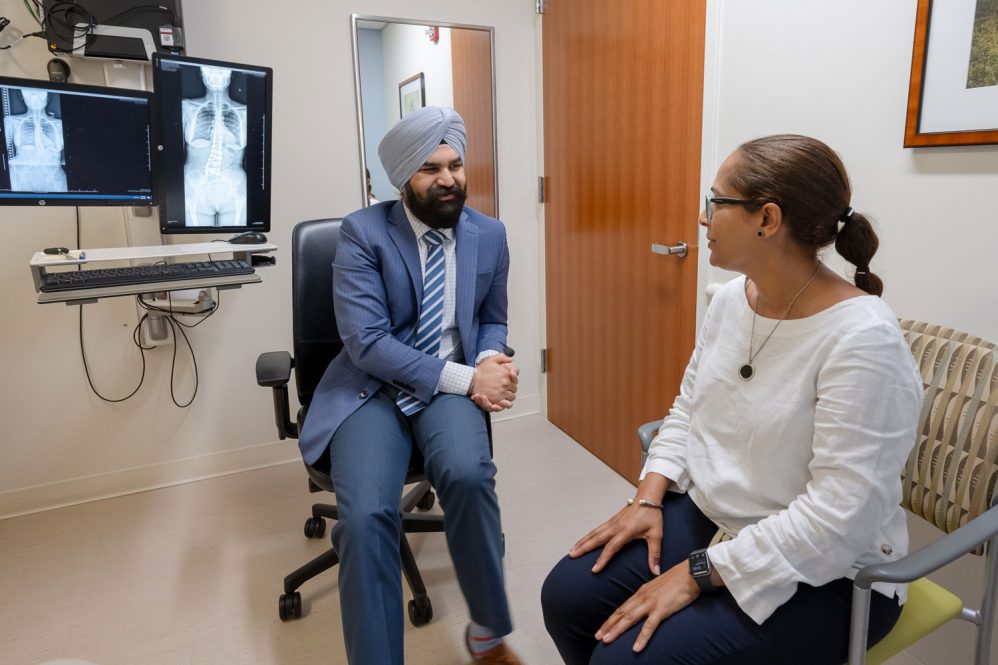
UConn Health spine surgeon Dr. Hardeep Singh uses devices fabricated to specific patient’s anatomy to perform spinal fusion
A relative few of the world’s spine surgeons are taking an advanced approach to correcting spinal deformities, one that uses imaging and 3D printing to fabricate implants custom to the patient’s anatomy.
One of them is Dr. Hardeep Singh from UConn Health’s Comprehensive Spine Center, the first surgeon in Connecticut to execute a multilevel lumbar fusion with patient-specific interbody devices.

The patient, Edurne Heredia of Manchester, calls the results “amazing.”
“It was at the point I couldn’t handle the pain anymore,” says Heredia, who, it turns out, had been dealing with a severe curvature in her lower spine for decades. “Nothing worked. I tried everything.”
That included physical therapy, injections, even a nerve block. She was advised she’d need to find a specialist in New York or Boston, but the pandemic kept her from traveling. She eventually found her way to Singh, who diagnosed her with hemivertebrae early last year.
“I couldn’t do anything in the house; I couldn’t even do the dishes anymore because of the pain,” Heredia says. “So I said, ‘Yeah, let’s do it. I’m in God’s hands and in your hands, Doctor.’ And I did it.”
Her spinal deformity was tilting her to one side. The spaces between her lower vertebrae were a pronounced wedge shape. Standard implants could work, but were not optimal.
“Typically, this deformity would be addressed by resecting the hemivertebrae and realigning the spine to its native state,” Singh says. “However, it requires a larger invasive procedure with significant risks involved.”
It made Heredia a candidate for a customized solution, using four asymmetric implants designed specifically to fit her anatomy, rather than altering her anatomy to fit standard implants.
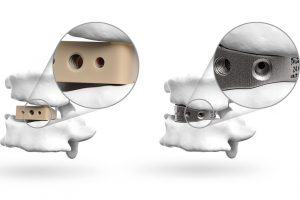
“This technology allows us to design implants that fit the topography of her spine and allows for a more natural correction of her deformity,” Singh says. “The surface of the implant is designed such that it mimics the microarchitecture of bone, allowing bone to grow onto the implant as well as through it, thus, providing the stability needed for a fusion.”
The procedure itself is largely similar to a traditional lumbar fusion with “off-the-shelf” implants.
“Deformity correction such as this is still a large undertaking, however, this approach provides us with the ability to address each patient’s spinal pathology in a more patient-specific way,” Singh says.
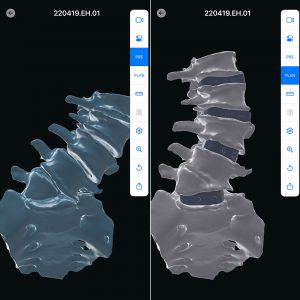
For that, Singh works with California-based Carlsmed to design the patient-specific implants based on the requirements for the patient and the patient’s anatomical images. The process involves generating a three-dimensional model which allow the spinal deformity to be fully visualized and each implant can be specifically designed to provide the correction needed.

“This provides us with the ability to analyze the spinal deformity in a 3D model, understand the drivers of the deformity, and design patient-specific implants which perfectly match the contours of the bone and serve to provide the correction desired,” Singh says. “The benefit is that it is customized to the patient’s anatomy and prevents any undue stress on the vertebral bodies as would be the case with standard implants. Before even entering the operating room, you have a visual of what the ultimate result will look like and this gives you the ability to modify the plan according to the patient’s needs.”
The visual preview comes with the added benefit of helping patients better understand the procedure and its benefits. They are able to go through the model with their surgeon and understand exactly what will be done and what the ultimate outcome will look like.
“As a spine center, our core philosophy is to individualize all our treatments to each patient’s particular circumstances, anatomy and pathology,” says Dr. Isaac Moss, chair of UConn Health’s Department of Orthoepedic Surgery and co-director of the Comprehensive Spine Center. “Technology, such as these custom-printed implants, allows us to take our personalized care to the next level.”

Carlsmed’s 3D-printed titanium “aprevo” devices have earned “Breakthrough Device” designation from the Food and Drug Administration.
Heredia, who turns 52 in November, has been working in customer service at the American Airlines counter at Bradley Airport since 1995. It’s a job that requires her to be on her feet all day, and one that constantly reminded her of her discomfort. Missing work for recovery and rehabilitation is taking some adjusting, as does having to scale back her roles outside work as a wife, mother, daughter, and sister.
“I was always the first one there, but I can’t do it anymore because I’m in pain all the time,” Heredia says. “I want to take care of everybody else, but if I want to do that, I have to take care of myself.”
Now, 14 months after the surgery, things have improved, but there is still a long road ahead.

“The pain is easier,” Heredia says. “It has been reduced. My back is straight. If I’m standing up, you don’t see the bump in my back. It was a bump in the left-hand side of my body. Now, I’m straight. My hip is straight.”
And while she still has more healing to do and limitations to stay within, Heredia says, “I’m happy with my decision to have this procedure.”
Learn more about the Comprehensive Spine Center at UConn Health.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com