A group of Korean researchers conducted a retrospective study to establish the efficacy and safety of patient-specific 3D printed titanium implants on the maxillofacial bones.
More from the News
During the study, a total of 16 patients were observed, each of them was undergoing reconstructive surgery for various maxillofacial abnormalities. The patients were equipped with customised titanium implants and had long-term follow-ups over a period of several months.
Only one of the 28 implants used failed to bond properly with the bone, while the others showed “acceptable” results in the treatment of various oral and maxillofacial abnormalities.
Maxillofacial implants printed in 3D
3D printing has long been used to construct guides that enhance patient outcomes, but it has only just begun to be employed on an experimental basis to create face grafts that may be transplanted into patients’ skulls. Scientists at Texas A&M University, for example, have developed a unique 3D printed scaffold that promotes bone cell proliferation following surgery.
In terms of other applications, the Québec Industrial Research Centre (CRIQ) has used a GE Additive Arcam Q10 3D printer to speed up the production of patient-specific lower jawbone implants, while Paulista University researchers 3D printed a facial prosthetic for a Brazilian cancer survivor that included her entire right eye.
Recently, Health Canada approved the first 3D printed medical implant created in Canada, a customisable mandibular plate to be used in face reconstruction surgery, primarily for patients with mouth cancer.
Retrospective investigation
Although autogenous bone grafting or implant insertion is the initial option for treating oral and maxillofacial abnormalities, there may be issues with donor-site morbidity, surgical failure, and reoperation.
Rapid advancements in digital technology have opened up new paths in the field of oral and maxillofacial surgery, with 3D printing allowing for faster and more precise surgical operations, particularly with titanium materials that have previously been proven to be biocompatible as dental implants.
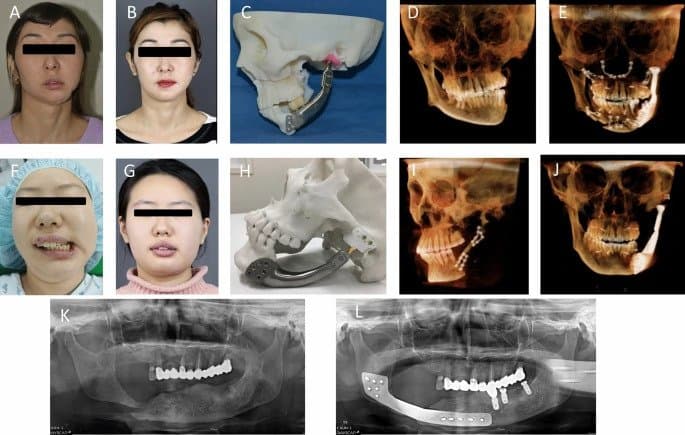
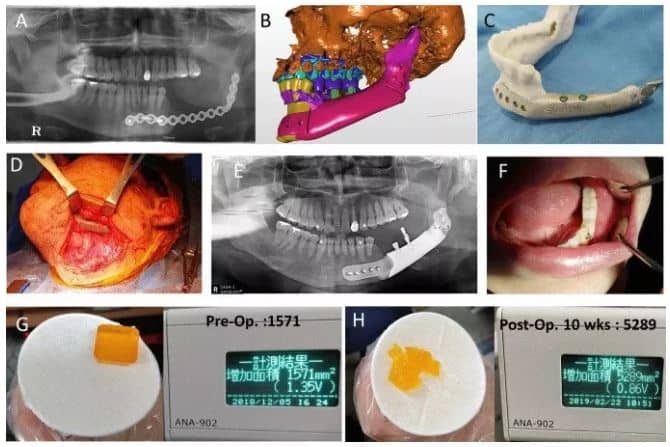
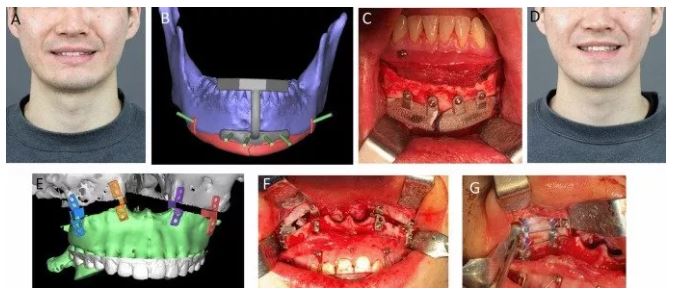
The maxillofacial titanium implants utilized in the surgical procedures documented in the study were 3D printed using electron beam melting (EBM) and selective laser sintering (SLS). In all, 28 implants were 3D printed and implanted into the maxilla (dominant region of the face), mandible (lower jaw), or zygoma (cheek/temple) of 16 distinct patients.
The patients in question, seven of whom were female and nine of whom were male, varied in age from nine to 78. Five mandibular segments, nine zygomas, ten mandibular our bodies, angles, or chins, and four maxillary sections were among the 28 faulty sites that were operated on.
After that, a long-term follow-up program was implemented, ranging in length from eight to 79 months per patient. The study focused on the titanium implant body’s bone fusion, but it also recorded postoperative infection, implant malunion, helpful results, patient satisfaction, subsidence, osteolysis throughout the implants, and any issues that developed.
Only one of the 28 implants failed to fuse with the bone, according to the study. A CBCT scan revealed that 96.5 percent of bone fusion had occurred six months following surgery. There was also no evidence of osteolysis – a degenerative condition in which bone tissue is damaged – or sinking around the titanium implants, according to the study.
According to the study, the patients who participated in the experiment were generally pleased with the aesthetically and functional outcomes of their surgery. However, two of the five patients who had a cheekbone restoration had revision surgery due to dissatisfaction with the implant’s appearance.

Examination of the implants
The bone-to-implant interface of the 3D printed implants was designed as either a mesh or a stable interface, depending on whether or not stability was necessary. This one was the most popular because the mesh titanium implant’s rough surface was proven to be more likely to mix with the patient’s bone.
SLS allows additive manufacture of metals such as titanium at high sintering temperatures; however, because to limited dimensional precision and poor surface roughness, process improvements are being undertaken to improve its capabilities. In order to sinter or fuse the supply, EBM uses an electron beam rather than a laser beam. In contrast to SLS, EBM may be used to fabricate sophisticated geometries by selectively scanning each cross-sectional layer.
Although the implants 3D printed with EBM were more expensive than those 3D printed with SLS, there was no difference in the scientific findings based on the kind of implant interface or the 3D printing technology.
Three of the 16 patients experienced screw fractures and aesthetic dissatisfaction at follow-up sessions, but all of these issues were eventually rectified, and post-operative restoration was found to be acceptable in all patients.
The study has provided recommendations for the use of 3D printed titanium patient-specific implants based on the patients’ experiences. In the short term, the study recommends that such implants be used for continuity defects of the facial bone limited to hard tissue for which reconstruction has already been performed and for which there is no reconstruction option, as well as for instances where there is a delicate or reasonable bone defect as a result of previous extreme bone preparation in a patient with facial osteoplasty.
Furthermore, the criteria state that 3D printed titanium implants must be used in cases of high cosmetic demands, such as correcting skeletal asymmetry, for locations that require functional load bearing, such as the jaw, and when dental implants must be used simultaneously.
Further data on the research could be discovered within the paper titled: “Reconstruction of maxillofacial bone defects using patient-specific long-lasting titanium implants,” printed within the Nature journal. The research was co-authored by H. Lim, Y. Choi, W. Choi, I. Song, and U. Lee.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com/