A breakthrough technique developed by University of Oxford researchers could one day provide tailored repairs for those who suffer brain injuries. The researchers demonstrated for the first time that neural cells can be 3D printed to mimic the architecture of the cerebral cortex. These results have been published today in the journal Nature Communications.
Brain injuries, including those caused by trauma, stroke and surgery for brain tumours, typically result in significant damage to the cerebral cortex (the outer layer of the human brain), leading to difficulties in cognition, movement and communication. For example, each year, around 70 million people globally suffer from traumatic brain injury (TBI), with 5 million of these cases being severe or fatal. Currently, there are no effective treatments for severe brain injuries, leading to serious impacts on quality of life.
This advance marks a significant step towards the fabrication of materials with the full structure and function of natural brain tissues. The work will provide a unique opportunity to explore the workings of the human cortex and, in the long term, it will offer hope to individuals who sustain brain injuries.
Lead author Dr Yongcheng Jin (Department of Chemistry, University of Oxford)
Tissue regenerative therapies, especially those in which patients are given implants derived from their own stem cells, could be a promising route to treat brain injuries in the future. Up to now, however, there has been no method to ensure that implanted stem cells mimic the architecture of the brain.
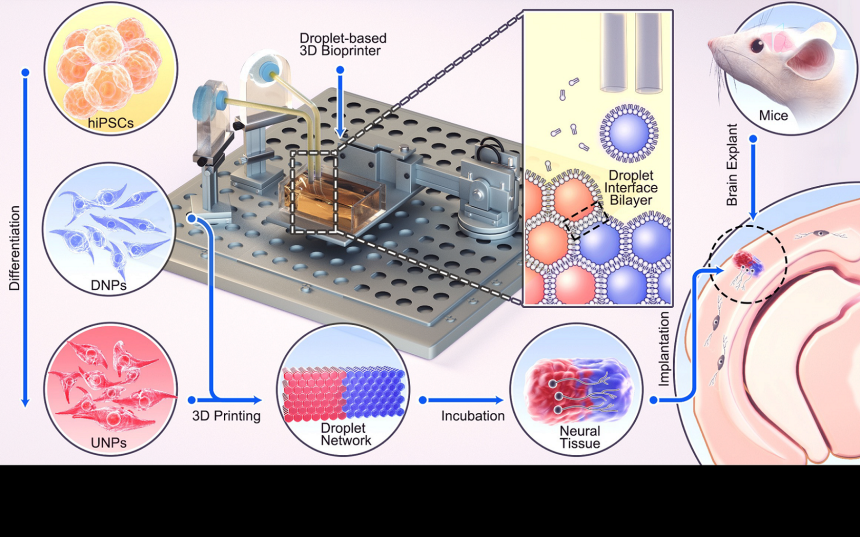
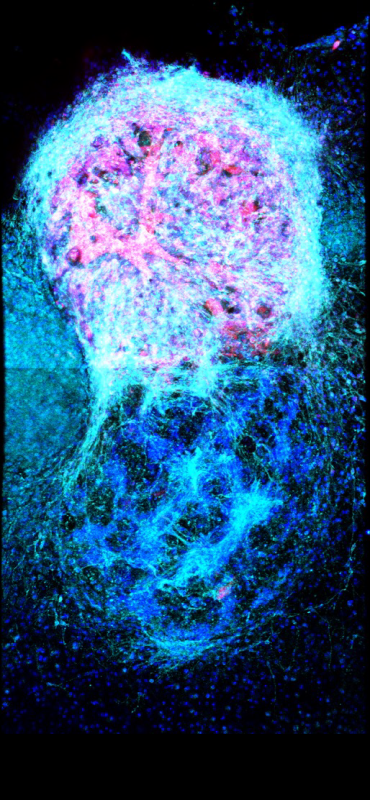
In this new study, the University of Oxford researchers fabricated a two-layered brain tissue by 3D printing human neural stem cells. When implanted into mouse brain slices, the cells showed convincing structural and functional integration with the host tissue.
The cortical structure was made from human induced pluripotent stem cells (hiPSCs), which have the potential to produce the cell types found in most human tissues. A key advantage of using hiPSCs for tissue repair is that they can be easily derived from cells harvested from patients themselves, and therefore would not trigger an immune response.
The hiPSCs were differentiated into neural progenitor cells for two different layers of the cerebral cortex, by using specific combinations of growth factors and chemicals. The cells were then suspended in solution to generate two ‘bioinks’, which were then printed to produce a two-layered structure. In culture, the printed tissues maintained their layered cellular architecture for weeks, as indicated by the expression of layer-specific biomarkers.
When the printed tissues were implanted into mouse brain slices, they showed strong integration, as demonstrated by the projection of neural processes and the migration of neurons across the implant-host boundary. The implanted cells also showed signalling activity, which correlated with that of the host cells. This indicates that the human and mouse cells were communicating with each other, demonstrating functional as well as structural integration.
The researchers now intend to further refine the droplet printing technique to create complex multi-layered cerebral cortex tissues that more realistically mimic the human brain’s architecture. Besides their potential for repairing brain injuries, these engineered tissues might be used in drug evaluation, studies of brain development, and to improve our understanding of the basis of cognition.
The new advance builds on the team’s decade-long track record in inventing and patenting 3D printing technologies for synthetic tissues and cultured cells.
Senior author Dr Linna Zhou (Department of Chemistry, University of Oxford) said: ‘Our droplet printing technique provides a means to engineer living 3D tissues with desired architectures, which brings us closer to the creation of personalized implantation treatments for brain injury.’
Senior author Associate Professor Francis Szele (Department of Physiology, Anatomy and Genetics, University of Oxford) added: ‘The use of living brain slices creates a powerful platform for interrogating the utility of 3D printing in brain repair. It is a natural bridge between studying 3D printed cortical column development in vitro and their integration into brains in animal models of injury.’
Senior author Professor Zoltán Molnár (Department of Physiology, Anatomy and Genetics, University of Oxford) said: ‘Human brain development is a delicate and elaborate process with a complex choreography. It would be naïve to think that we can recreate the entire cellular progression in the laboratory. Nonetheless, our 3D printing project demonstrates substantial progress in controlling the fates and arrangements of human iPSCs to form the basic functional units of the cerebral cortex.’
Senior author Professor Hagan Bayley (Department of Chemistry, University of Oxford) said: ‘This futuristic endeavour could only have been achieved by the highly multidisciplinary interactions encouraged by Oxford’s Martin School, involving both Oxford’s Department of Chemistry and the Department of Physiology, Anatomy and Genetics.’
The study ‘Integration of 3D-Printed Cerebral Cortical Tissue into an ex vivo Lesioned Brain Slice’ has been published in Nature Communications.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com