The researchers at Brisbane Royal and Women’s Hospital (RBWH), uses FDM technology and 3D scanning to predict radiation damage in patients by developing prototypes. The 3D printed prototypes helps doctors to find appropriate dose of radiation for patients.
Key points:
- Researchers say the technology will make radiation safer for cancer patients
- More than 100 skin cancer patients have been treated with 3D printing devices
- Tanya Kairn says the technology has already been “revolutionary” for her patients
Reducing radiation pain among skin cancer patients
The institute has used 3D printing to optimise radiation treatment for skin cancer. Without a manufactured layer being placed on the skin, radiation levels can build up in the underlying flesh and have little effect on the skin. “For a patient with skin cancer, what we want is to be able to treat the skin where the cancer is, and also be able to treat the underlying tissue where the cancer has invaded,” Dr Kairn said. This layer is called a “bolus”, which is made from wax and other materials and has been used for decades. Dr Kairn said 3D printing has made a “huge difference” to the pain experienced by skin cancer patients. To demonstrate, Dr Kairn held up two red nose moulds, as well as two oddly shaped blue moulds made for people whose faces have been eaten away by cancers.
Dr Kairn said eliminating the need for a health professional to physically touch patients’ “painful, inflamed cancerous tissue” to form a mould has been “revolutionary”. “We’ve treated over 100 patients using these types of devices,” she said. While face cancers are a common use for the technology, it can be used on any part of the body with an external cancer.
On the upper levels of an inconspicuous building on the Brisbane Royal and Women’s Hospital (RBWH), 3D printing technology is creating products that may one day save your life. The Herston Biofabrication Institute says it is the first organisation in Australia that brings doctors, engineers and academics together to focus on the many medical uses of 3D printing. Printers slowly build up layers of resin to create a desired body part for cancer patients.
“The goal was very much to support that coordination of engineers and researchers with clinicians and consumers on one site,” General Manager Mathilde Desselle said.
Plastics that act like human tissue
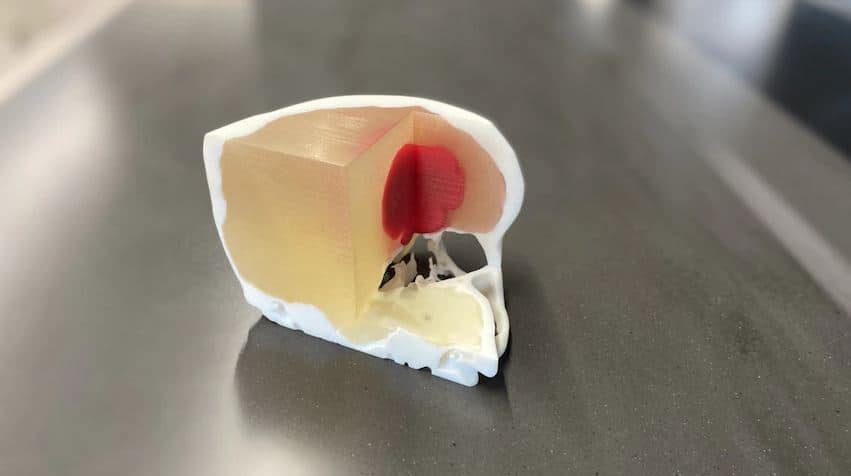
RBWH Director of Medical Physics in Cancer Care, Tanya Kairn already knows how meaningful this technology could be for patients. She said the use of 3D printing technology has been “revolutionary” for her patients. A model human head has the eyes of someone who has faced radiation one too many times. The head comes apart in layers, showing different densities and patterns.
Dr Kairn said technology like this has been used to measure radiation doses for specific patients to make treatment safer. “We can calculate that dose, and we can predict that dose, but we can’t measure it,” she said. “So, what we need is a really good replica of the patient, that includes all these different densities.”
While the work of Dr Kairn deals with external radiation, Senior Medical Physicist Rachael Wilks deals with radioactive sources inside the body. Dr Wilks has been working on a clinical trial that utilises 3D printed moulds to treat “a whole range of gynaecological cancers” using brachytherapy. Brachytherapy is the insertion of radioactive material inside the body and is sometimes known as internal radiation. It targets tumours directly and is often used in combination with external treatments. “Instead of electronic photons just bombarding from every angle, it’s specifically a little itty bitty radioactive source about four millimetres long, one millimetre diameter,” Dr Wilks said. Usually, brachytherapy is delivered via cylinders that vary in diameter. Dr Wilks said most patients can be treated with these cylinders, but problems can arise from the fact that “patients aren’t cylinders with different diameters”. She said there were existing custom mould techniques, but they were “imprecise” and took multiple efforts. “This is a way to do it once. So, a lot of time savings and material savings as well,” she said. “It enables this brachytherapy to be delivered to patients that would otherwise never have .” The current clinical trial involves 10 patients with the goal of expanding it so the technology can be made available to more patients.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com/