Additive manufacturing, popularly known as 3D printing, has emerged as a game-changer in various industries, spearheading the third industrial revolution by fundamentally reshaping manufacturing processes. Historically, the production of functional products involved complex and time-consuming steps. However, additive manufacturing has revolutionized this landscape, allowing for the direct fabrication of functional items from raw materials in a fraction of the time previously required.
The implications of this innovation are far-reaching, with its influence spanning across sectors such as automotive, aerospace, electronics, and notably, healthcare. Within healthcare, additive manufacturing holds immense promise for producing bespoke, patient-specific implants with unparalleled precision and accuracy. Applications extend to implantable heart valves, rib cages, osseous structures, and beyond.
The versatility of additive manufacturing shines through its ability to handle an extensive array of materials, including ceramics, metals, polymers, and composites. This capability enables the fabrication of intricate implants tailored to the nuanced needs of individual patients.
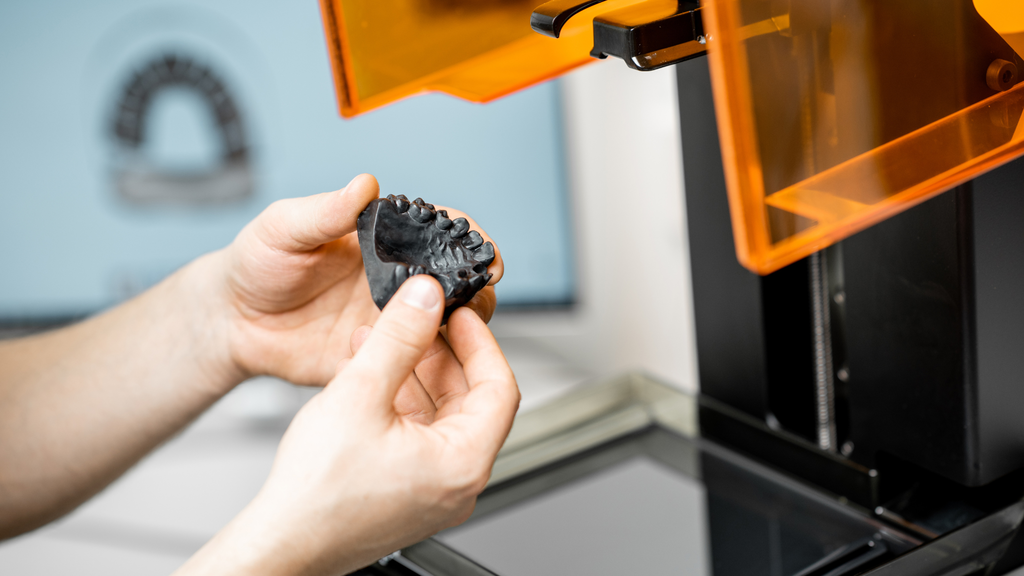
In dentistry, additive manufacturing plays a pivotal role, facilitating the creation of maxillofacial implants, dentures, and prosthetic adjuncts with heightened precision and customization. Furthermore, its utility extends to surgical training and planning, where the facile generation of anatomical models through additive manufacturing streamlines preparatory endeavors.
Advancements in Imaging and Reconstruction
Various imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), provide three-dimensional models of organs essential for designing personalized implants. The post-processing of images using software like MIMICS allows for the creation of implant features tailored to individual anatomical requirements.
Three-dimensional printing involves stacking images obtained from imaging techniques to construct a structure, a process known as tessellation. This method allows for the fabrication of models layer by layer, with each layer’s thickness determining the dimensional accuracy along the vertical axis. The materials used in 3D printing can be fabricated to form hollow, semi-solid, or solid structures, offering flexibility in design and function.
Applications in Reconstruction and Orthognathic Surgery
Maxillofacial trauma and tumors often necessitate precise surgical intervention. 3D printing has revolutionized preoperative planning and surgical simulations, offering superior accuracy compared to traditional methods. Studies show that stereolithographic technology significantly enhances diagnostic and operative precision, reducing operation time while improving outcomes.
In orthognathic surgery, various 3D-printed surgical guides and templates enhance surgical accuracy and efficiency. Customized surgical guides minimize deviations and reduce surgical times, ensuring optimal occlusion and patient satisfaction. Optimized protocols utilizing 3D planning and printing have improved surgical accuracy and efficiency in bimaxillary orthognathic surgery.
Maxillofacial implants
In some cases, patients suffer fracture of the chin and jaw Owing to trauma. In other patients, cancer may spread to a Region of the jaw and the infected tissue needs to be Removed. Three-dimensional printing may be applied to Replace the entire jaw or a portion of the jaw.50,51 As Observed in Figure (5 and 3)D printed metallic implants to Replace the jaw may be created. This is done through a Powder metallurgy based AM process known as selective Laser melting (SLM). In this process, the powdered form of The metal is melted and fused to the previous layer, thereby Creating a three-dimensional object. The implant created is a bioinert one that remains inert and does not undergo any changes when reacted upon by bodily fluids. The implant was created using powdered titanium.
Bioresorbable maxillary and mandibular implants using calcium phosphates have also been fabricated.39,40,52 The implant is made either by dissolving the material in a photo curable mix and allowing the implant to set in the presence of a suitable light39 or by mixing the material with a suitable binder and allowing the implant to dry.40 In this pro-cess, the layers of calcium are bound to each other by means of a strong binder or glue that holds the layers together. Calcium phosphates are commonly found in the body. As a result, the implant is bioresorbable in nature and eliminates the need for an immunosuppressant. Similar studies have been conducted using 7 phosphate and hydroxyl apatite53 for bone reconstruction and favorable results such as integration of the implant into the native tissue have been observed.
Utilization in Working Models and Complete Dentures
In digital dentistry, 3D printing is commonly utilized to construct dental arches, replacing physical gypsum models prone to loss and damage. Compared to traditional plaster models, 3D printed models offer numerous advantages including lighter weight, enhanced durability, and utilization of digital data.
3D printing technologies enable the direct creation of complete denture resin bases from CAD data, eliminating the need for molds or cutting tools. The accuracy of complete denture bases is crucial for masticatory performance and retention. Studies show that denture bases fabricated using photopolymerization spray or CAD/CAM techniques exhibit superior accuracy compared to conventional methods like thermal polymerization.
Advancements in Removable Partial Denture (RPD) Frames and Occlusal Splints
Rapid advancements in CAD/CAM technology have transformed the fabrication process of removable partial denture (RPD) frames, offering personalized solutions and improved patient outcomes. The streamlined approach involves scanning either intraorally or extraorally using advanced scanners, transferring digital files to CAD software for precise design, and fabricating RPD frames with remarkable accuracy and efficiency using 3D printers.
The occlusal splint, an intraoral device targeting temporomandibular joint disorders, benefits from 3D printing’s efficiency and cost-effectiveness. While concerns regarding material durability persist, 3D-printed splints demonstrate satisfactory performance within a clinical timeframe.
Custom Tray Manufacturing and Future Prospects
Accurate implant impressions are crucial for effective prosthesis manufacturing, with 3D-printed custom trays offering heightened precision and reproducibility compared to traditional methods. Clinicians favor 3D-printed custom trays due to their personalization and precision, suggesting wider adoption in implant tray manufacturing.
Tooth-supported crowns and fixed dental Prostheses (FDPs)
AM technologies to fabricate metal frameworks were also introduced for tooth-supported crowns and FDPs; however, the only metal available in dentistry today is CoCr alloy . DMLS porcelain fused metal crowns alloys can be processed using AM technologies Different studies have analyzed the marginal and internal discrepancy of AM metal framework as well as the Ceramic bond strength of 3D-printed metals. Most studies report a clinically acceptable marginal and internal fit as well as a metal-ceramic bond strength comparable to conventional casting methods. The ceramic bond strength of AM CoCr metal alloys has also been reported to be superior to the current standards of ceramic bond strength, surpassing the minimum acceptable strength of 25 MPa required by AINSA/ADA specification No. 38 (2000) and ISO 9693:1999(E) using the three-bending test
AM technologies showed comparable and adequate capabilIties to accurately translate STL file data into frameworks.
Tissue engineering
Tissue engineering is the process through which native tisSue is generated by using a combination of cells and materials. The cells may be deposited on a 3D structure known as a scaffold (scaffold-based tissue engineering) or may be allowed to proliferate without a scaffold (scaffold-less tissue Engineering). In scaffold-less tissue engineering, polymeric materials are required to construct support structures for the movement of blood and nutrients. Direct printing of cells to form functional tissues, thereby eliminating the need of a scaffold is also being researched upon. Cells in the form of spheroids may be deposited layer by layer. This application may be used in dental tissue regeneration, where the pulp cavity may be filled with cells in a preset pattern and microstructured biomaterials. Here, the necessity for a scaffold is eliminated as the scaffolds have been arranged in a pattern and do not require a scaffold to facilitate the arrangement and stabilization of cells. Hydrogels may be used as carriers to enable the deposition of cells. In this process, bioinks comprising cells, media, and other stabilizing agents are used in lieu of plastics and other materials used in printing. While 3D printed tissue engineering is still in its nascent stages of development, the applications are many and cannot be ignored.
Benefits of additive manufacturing in dentistry
In dentistry, there are various requirements for the patients; such as crown, implants and bridges. Various AM technologies are beneficial for dentistry. Binding jet technology is used to manufacture dental prostheses. Various parameters are taken such as drying powder level, binder amount, drying time and powder spreading speed. The result shows that it provides an accurate implant with low cost and better strength.Additive manufacturing is used to manufacture patient specific eruption guidance appliances, thereby increasing patient comfort and reducing overall cost of the model. Binding Jet 3D printing technology is used to produce partial denture by using metallic powder. Micro-computed tomography is used to scan the existing framework for obtaining a 3D printed model. The result shows that it helps to achieve more than 99% density with controlled shrinkage at a lesser cost. It is highly compatible to produce complex shape dental implant with exact dimensions.33 The comparison of the accuracy of dental restoration manufactured through additive manufacturing and subtractive manufacturing method using wax or zirconia milling is undertaken. The result shows that the accuracy of dental restorations manufactured by additive manufacturing technique is higher than that of subtractive methods. AM is also a digital method which stores inventory in digital form; as a result, it also reduced inventory cost. The experimental analysis for dimensional accuracy is done for teeth manufactured by FDM technique. The intraoral 3D scanner is used to create a 3D digital model and manufactured model by three different layer thicknesses. Dimensional accuracy of the model is evaluated by GOM Inspect software, which shows that the reducing layer thickness easily achieves a high level of accuracy . Additive manufacturing fulfils the customised requirements of dentistry in lesser time and cost.
Following are the significant benefits obtained through the adoption of 3D Printing in Dentistry:
- Faster and accurate service
- Cost-effective
- Determine depth and width of teeth
- Easily fabricate customised implants
- Reduce fabrication time
- With its digital storage, there is considerable inventory reduction of physical models
- Rapidly produce custom design
- Accurate sizing for implantsBenefits of additive manufacturing in dentistry
Drawbacks
Not all materials can be processed by AM; certain materials may not be completely compatible. As a result, it becomes difficult to fabricate them. Replacement materials may or may not be as suited or as Competent as their predecessor materials. Also, cost is a major factor as specialized machinery costs a lot. While AM by itself consumes less time, prefabrication and postprocessing may be intensive.
Future scope
In future, AM can print low-cost, functional dentures using multiple biocompatible materials. It can give a fully printable denture solution. AM is rapidly evolving with new materials. Prosthodontics physical models and any customised, low-cost dental implants seem to be viable. AM technologies can enable collaboration among clinician and laboratory and help to provide a perfect solution for the production of various types of customised medical and dentistry models. In conclusion, the integration of 3D printing in Dentistry promises a paradigm shift in patient care, characterized by bespoke solutions and enhanced precision. As technology continues to advance, the future holds even greater potential for innovation and transformation in dental healthcare. Owing to the recent advancements in technology, it is believed that AM will play a greater role in healthcare in General and dentistry in particular in the near future.
Subscribe to AM Chronicle Newsletter to stay connected: https://bit.ly/3fBZ1mP
Follow us on LinkedIn: https://bit.ly/3IjhrFq
Visit for more interesting content on additive manufacturing: https://amchronicle.com